Background: Preterm born infants are at an increased risk of developing iron deficiency (ID) despite preventative iron supplementation, which can lead to long-term negative neurodevelopmental and behavioral outcomes. Serum ferritin (SF) is the commonly used test for diagnosing ID. However, SF is influenced by infection and inflammation, making it an unreliable marker in such situations. An alternative, reticulocyte hemoglobin equivalent (Ret-He), measures the iron content in newly produced red blood cells, providing an immediate assessment of iron availability. Unlike SF, Ret-He tests are automated, can be performed on the same blood sample as a complete blood count, and is not influenced by infection or inflammation like SF. However, there is limited literature on the reliability of Ret-He as an ID marker in very preterm infants (VPI) during their first year of life. This study aims to evaluate the diagnostic accuracy of Ret-He as an ID indicator in VPI at 4-6 months of corrected age (CA) compared to SF levels.
Objective: To investigate the accuracy of Ret-He in detecting ID in VPI at 4-6 months CA
Methods: A retrospective population-based cohort study was conducted using a population-based Provincial Perinatal Follow-Up (PFUP) database on all live VPIs born in Nova Scotia between 2012 and 2018. Infants with hematological disorders, chromosomal abnormalities, or major congenital anomalies were excluded. Prophylactic iron supplementation (2-3 mg/kg/day) starting at 2-4 weeks of chronological age was a standard of care for all included infants. Iron supplementation was recommended until 9-12 months CA. All infants underwent SF and CBC testing at either 4- or 6-months CA to assess iron stores and guide supplementation. In 2012, Ret-He was added as an additional marker of ID for clinical decision-making. Two definitions of ID were used. Definition one defined ID as SF level <20 mcg/L. Definition two defined ID as SF level <20 mcg/L at 4 months and <12 mcg/L at 6 months CA. Receiver operating characteristic curves were performed and the areas under the curves (AUC) were calculated to assess the accuracy of Ret-He in classifying patients with ID. The optimal cut-off point for Ret-He was determined using Youden's index, from which sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. The Spearman correlation coefficient was calculated between SF and Ret-He. Statistical significance was set at a two-sided P value of < 0.05.
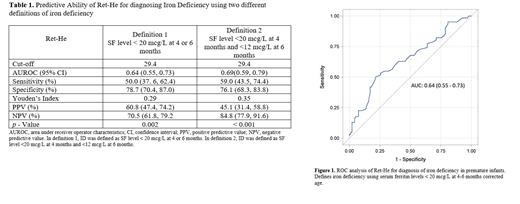
Results: A total of 156 patients were included. Under definition one, 62 (39.7%) met the criteria for ID. Under definition two, 39 (25.0%) patients had ID. Baseline characteristics are provided in Table 1. The Spearman correlation coefficient between SF and Ret-He was 0.23 (p=0.004). Under definition one, the AUC of Ret-He for diagnosing ID was 0.64 (p=0.002) and 0.69 (p<0.001) under definition two (Figure 1). The optimal cut-off value for Ret-He in ID diagnosis was 29.4 pg irrespective of the definition. Sensitivity, specificity, PPV, and NPV for both definitions are reported in Table 1.
Conclusion: Regardless of the ID definition used, the AUCs indicated a weak discriminatory ability of Ret-He for ID diagnosis. The study indicated a weak positive relationship between SF and Ret-He. Ret-He's low diagnostic accuracy in this study is comparable to other studies involving healthy pediatric populations but lower than studies involving children with chronic health conditions. Clinicians should use caution when relying on Ret-He alone to diagnose ID in VPI. Further research is needed to determine the optimal diagnostic approach for identifying ID in VPI as well as explore the clinical utility of Ret-He in combination with other ID biomarkers such as SF and transferrin saturation.
Disclosures
No relevant conflicts of interest to declare.